Complied by Walter Sorochan, Emeritus Professor: San Diego State University
Posted: June 21, updated November 24, 2021. Disclaimer The information presented here is for informative and educational purposes only and is not intended as curative or prescriptive advice. The statements of this web-site have not been evaluated by the United States Food and Drug Administration (FDA). Nothing stated here should be considered as medical advice for dealing with a given problem, or to diagnose / treat / prevent / cure any disease.
This article deals with prostate enlargement or BPH and Urinary Retention. Although this article primarily addresses lower urinary tract voiding [urination] dysfunction in men, it also briefly touches on women who may have voiding symptoms that are similar to men. The contents of this article are what every man and woman needs to know. This article is intended as information for non-medical persons.
 Boys and young men are especially aware of their ability to project a strong
urine stream. Bragging rights on who can pee stream the farthest!
Normally all is well until the prostate, about the size of a walnut,
begins to naturally enlarge. At middle age, urination ability
often changes, with males often urinating more frequently and with less
force.
Boys and young men are especially aware of their ability to project a strong
urine stream. Bragging rights on who can pee stream the farthest!
Normally all is well until the prostate, about the size of a walnut,
begins to naturally enlarge. At middle age, urination ability
often changes, with males often urinating more frequently and with less
force.
What has happened is that the prostate gland has continued to grow, causing enlargement of the prostate gland. As men age, four main types of prostrate problems can occur: enlargement of prostate, referred to as Benign prostate Hyperplasia [BPH]; urinary retention; prostatitis or infection/inflammation; and prostate cancer.
Video Length = 1:03 mns. Click refresh to
activate video
Source: What is BPH? Science Art
Incidence of BPH in USA & World: Benign prostate Hyperplasia [BPH] and its related complications is a very important problem. It has been estimated that the number of men with BPH in United States range from 12 million to over 20 million. The incidence is dramatically increasing, due to an increasing aging population in the United States. Although the medical community may be aware of the problem, the majority of men and women are not aware of this progressively-aging problem. Most men are not aware of this hidden but lurking problem. Also, health educators neglect to mention this as a major health problem that healthy males and females may face in later years.
Prostate enlargement in males is also a world problem and not just your or my or USA problem. Lower urinary tract symptoms [LUTS] are increasing in both ageing men and women. Thorpe: BPH 2003 Dmochowski: Bladder Outlet Obstruction 2005 According to the most commonly used measures of LUTS in epidemiologic studies by the American Urological Association Symptom Index [AUA] guidelines, there is an increase in the incidence of BPH worldwide. Globally, benign prostatic hyperplasia affected about 210 million males as of 2010 [6% of the population]. Vos: BPH in world 2012 WHO: BPH estimates 2009 Patel: Bladder obstruction review 2014 However, there is now a growing public health concern about BPH in India and Asian countries. Manchanda: Review Vit D therapy for BPH 2012 Bid: BPH concern for India 2008
So who gets BPH? Prostate enlargement, or benign prostatic hyperplasia [BPH] can start after the age of 40 and becomes more common as men get older. It affects nearly all men, though some men do not have any symptoms even though their prostate may have started to grow larger. More than half of men in their sixties and as many as 90 percent of men in their seventies and beyond exhibit some symptoms of BPH.
"BPH [prostate enlargement] does not necessarily constitute a problem to many men. In fact, many men with histologic BPH will never see a doctor for this condition, nor do they ever need any treatment for it. The condition becomes a medical problem if and when it is associated with subjective symptoms, the most common being lower urinary tract symptoms [LUTS] or urine retention." Roehrborn: BPH overview 2005 This observation by Roehrborn is important as men may have weak symptoms that appear to present no urination problems initially but eventuate into urination complications later on.
In women, iatrogenic [medical] causes of obstruction are the most common. Although the BPH in women may be somewhat different from men due to anatomical differences, the communication problems between the GP and women are similar to those with men. Given the unique male and female differences in voiding, many of the prior urination analyses standardized for men do not apply to women. No urodynamic definition of obstruction in women has been generally accepted. Dmochowski reviews the urological approaches in dealing with the complexities of urine retention [obstruction] in women. Dmochowski: Bladder Outlet Obstruction 2005 Selner: Bladder Neck Obstruction 2016
The problem - Prostate enlargement and BPH etiology: What happens when the prostate gets larger? Prostate enlargement, or benign prostatic hyperplasia (BPH) is very common in men as they age.
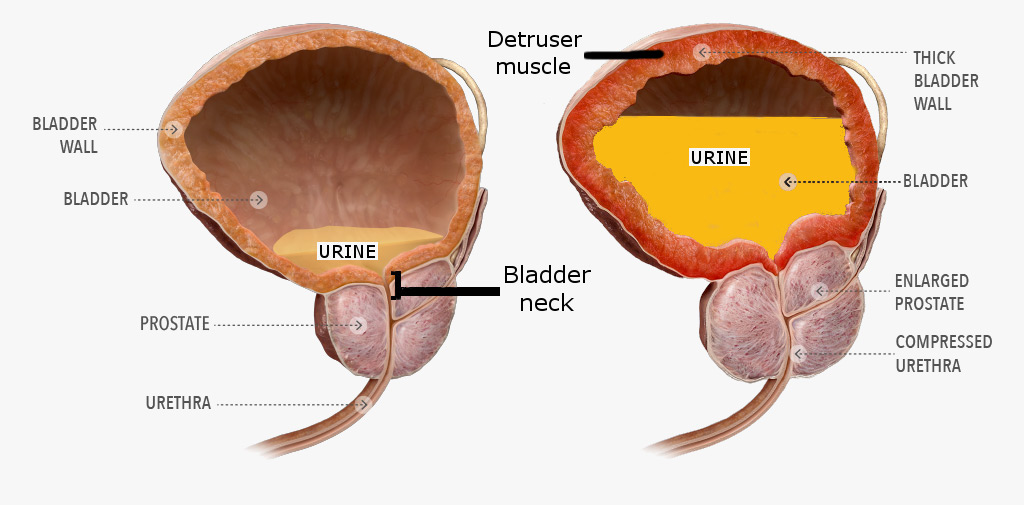
Illustration of normal prostate gland [on left] and
enlarged prostate gland on right.
Over time, the bladder muscle can become so weak that it can lose its ability to completely empty itself [above illustration on right]. As a result, the residual urine remaining in the bladder can act as a reservoir that harbors bacterial growth, leading to urinary tract infections (UTIs) and more seriously, potential kidney infections. As the prostate enlarges, the prostate begins to compress the urethra, blocking normal urine flow and often turning what was once a strong stream into a mere trickle [ above illustration on right side ]. In response to the increasing resistance to urine flow, the bladder walls can become irritated and begin to thicken. This results in the bladder contracting, even when it contains very little urine, resulting in a sudden and urgent need to urinate. In time, the growing need for frequent, urgent trips to the bathroom can become increasingly frustrating, especially when trying to get a good night’s sleep – or finish a round a golf. If left untreated, the enlarged prostrate gland and compressed urethra can block urination, causing urine retention.
|
Definition of symbols: Recent Terminological changes have led to the use of benign prostatic obstruction/enlargement (BPO/BPE) as nomenclature to replace previously used eponyms such as benign prostatic hyperplasia (BPH). BOO in men has traditionally been linked to the prostate. Also synonymous with BOO in men is LUTS. BOO may present as lower urinary tract symptoms (LUTS). The presence of moderate-to-severe LUTS is also associated with the development of acute urinary retention (AUR) as a symptom of BPH progression. Dmochowski: Bladder Outlet Obstruction 2005 A study has estimated that 90% of men between 45 and 80 years of age suffer some type of LUTS. Article by McVary: Management of BPH is no longer active. |
Cause of BPH: Medical evidence suggests that there are genetic components to both BPH and LUTS. Investigators further estimated that of the 50% of men undergoing surgery for BPH less than 60 years of age had an inheritable form of the disease. Patel: Bladder obstruction review 2014 Dmochowski: Bladder Outlet Obstruction 2005
Although extensive research on the impact of food and vitamin D on BPH is lacking at this time, recent research in India links vitamin D as a contributing cause. Manchanda: Review Vit D therapy for BPH 2012 This should not be a surprise as many persons now work indoors and seldom see the sunshine that, in turn, naturally activates the skin to synthesize vitamin D.
Recent evidence also suggests that estrogen hormonal actions via estrogen receptor subtypes also play an important role in BPH. Current pharmaceutical options for BPH have advantages, limitations and adverse effects. "Equol is a polyphenolic/isoflavonoid molecule derived from intestinal metabolism, dairy and dietary plant sources. Equol has potent anti-oxidant and anti-aging properties to decrease prostatic irritation and potentially neoplastic growth." Lephart: Cause of BPH 2014
Another possible cause is hormone 5-alpha reductase that converts testosterone to DHT, a potent stimulator of prostate growth that, in addition to being necessary for prostate development, appears to play a central role in BPH pathogenesis. Patel: Bladder obstruction review 2014
Many of the above factors may potentially be altered in order to delay onset, prevent progression or diminish symptoms.
Medical research about urinary problems and Communicable Disease Center [CDC] fail to mention that the American public is uninformed about urination in general. There is a need to step out of medical box and admit that such unawareness may be a real contributing factor to the urinary problems of middle-aged and senior citizens.
Recognizing Signs of BPH: Common symptoms of prostate enlargement tend to appear slowly and insidiously so that you probably won’t notice them until they’re pretty far along:
If you have one or more of the above signs, you need to see your medical doctor immediately!
Urine Retention or blockage: The presence of moderate-to-severe Urinary Tract Symptoms [signs] is associated with the development of acute urinary retention or inability to urinate! The patient will have an urgent need to urinate without being able to pass much urine.
Urine retention does occur in men and women, although most research articles focus on men. The most common urine retention in women is caused by surgery. Dmochowski: Bladder Outlet Obstruction 2005
What Is Bladder Neck Obstruction?: Bladder outlet obstruction is a blockage that slows or stops urine flow out of the bladder. Bladder outlet obstruction can cause urine to back up in your system, leading to difficult urination and other uncomfortable urinary symptoms.
The bladder neck is a group of muscles that connect the bladder to the urethra. [ refer to earlier illustration above] The muscles tighten to hold urine in the bladder, and relax to release it through the urethra. Urinary problems occur when abnormalities block the bladder neck and prevent it from opening completely during urination. Men over age 50 are more likely to develop bladder neck obstruction than any other group although Aggarwal reports that Primary bladder neck obstruction can be a rare condition of the lower urinary tract seen in young and middle-aged men and women. Aggarwal: Bladder neck obstruction update 2015 However, the condition can occur in both men and women at any age. Selner: Bladder Neck Obstruction 2016 This obstruction can also be caused by scars from surgery.
Although bladder neck obstruction is rare in women, it can develop when the bladder drops into the vagina. This usually occurs as a result of a weakened vaginal wall. The vaginal wall may become weak due to: Selner: Bladder Neck Obstruction 2016
There are surgical procedures to remedy bladder neck obstruction in women.
Persons unable to urinate need to go to the Emergency Room immediately. A medical doctor or nurse will insert a catheter, a flexible plastic tube, through the urethra into a bladder and empty the bladder, thus relieving the painful urge to urinate.
Then the patient will usually leave the emergency room with a temporary catheter in place, that allows the urine to drain from the bladder into a plastic bag attached to a leg. The bag has to be drained often to prevent infection.
Finally, an appointment needs to be made with a urologist; there may be a waiting time for a patient to see a urologist. A urologist will analyze the urine blockage and, with the patient, decide on the appropriate surgery and therapy.
Surgeries: Therapies for men and women are different. For men, there are many surgical therapies available, all of which require some form of anesthesia, be it spinal, epidural, or general. They differ in the energy employed and in the method by which tissue is incised, resected, or vaporized. The recommended surgical therapies are: Roehrborn: BPH overview 2005 Article by The Urology Group: Greenlight PVP is no loger active. Article by Payne: BPH treatment is no longer active
The reader can get more details on each surgical procedure by scrolling the internet or referring to the references.
The gold standard surgery in use since 1960 but refined since then is TURP!
Turp is done to treat symptoms as well as restore normal urethra function. For TURP, an instrument called the resectoscope is inserted through the urethra, the urinary pathway in the penis. The resectoscope is a fiber optic instrument that contains a tiny camera, allowing the surgeon to view the the prostate gland as the operation proceeds. The surgeon threads the resectoscope that also has an electrical loop, through the penis to the prostate area. The surgeon then uses one portion of the electrical loop to cut away the overgrown tissue that’s pressing against the urethra [ resection ]. During the procedure, the blocked portions of the urethra are opened up as the urethra is opened up.
During transurethral resection [remove excess prostate tissue] of the prostate (TURP), the surgeon uses one type of electrical current to chip away at the overgrown prostate tissue. The surgeon then applies a different electrical current to cauterize the tissue and reduce bleeding. The area is then flushed with a sterile solution to remove bits of tissue. A catheter is inserted temporarily into the urethra and bladder until the area recovers. After surgery, the newly enlarged passageway enables urine to flow more easily. Article by Loughlin: TURP options is no longer active The TURP procedure is illustrated below:
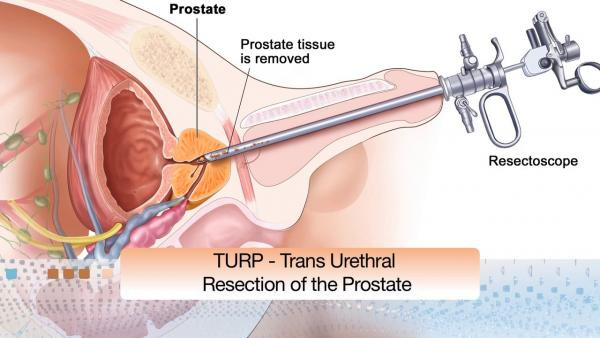
Surgical complications can occur. For example, if the surgeon does not remove and also clean out all the impacting prostate growth, then this left over debris can cause later urine retention and probably require another surgery in several years. Another complication can also occur should the surgeon 'roter root' away part of the urethral wall. Surgery may also leave a scare that can cause voiding problems. In some instances, the patient may have incontinence and need to wear a diaper.
Exercises to help strengthen bladder and other related urination muscles: When the muscles that control the bladder get weak, bladder exercises can help make them strong again. Doing bladder control exercises for just 5 minutes, three times a day, can make a big difference in your bladder control. If you have urination problems, you need to consult with your urologist and helper therapists to train you in the exercises that will strengthen your bladder muscles.
One of the exercises recommended for strengthening the bladder muscles are the Kegel exercises. Kegel exercises aim to strengthen pelvic floor muscles that support and hold up the bladder. When the pelvic floor muscles are weak, you are at greater risk for involuntary urine leaks. The value of improving urinary incontinence with Kegel exercises is now widely accepted. NAFC: Kegel exercises
Women -- How to Do Kegel Exercises: The video below is one way to learn how to do these exercises. Another approach is to view these Kegel illustrations and instructions.
Women: Kegel Exercises Beginners Workout by Michelle Kinway length=
10:59 mns
Drug therapy for BPH: For the past several decades, European doctors have routinely prescribed a variety of plant-based drugs to treat benign prostate enlargement and lower urinary tract symptoms. Although saw palmetto, pygeum, and nettle root extracts are common plant-based drugs prescribed to millions of men in Europe, research has discredited saw palmetto.
Beta-sitosterol is a plant fat contained in several European prostate drugs, though it is not routinely used in the United States. Multiple randomized studies have confirmed the efficacy of beta-sitosterol in alleviating the types of prostate discomfort that aging men so frequently encounter. Strum: Beta-Sitosterol 2005
Beta-sitosterol was effective in inducing apoptosis and inhibiting the growth BPH. Scientist Atif B. Awad and his team at the State University of New York at Buffalo have found that beta-sitosterol inhibits prostate and breast cancer cell growth, and induces cell cycle arrest. Awad: beta-sitosterol & BPH 2005
Strum and Faloon concluded, from European studies, that phytochemicals may induce the inhibition of tumor growth by stimulating apoptosis and arresting cells at different locations in the cell cycle, and that the mechanism may involve alterations in ROS (reactive oxygen species) and prostaglandin production. Strum: Beta-Sitosterol 2005
For millions of men in American, benign prostate enlargement will severely downgrade their quality of life. Yet across the ocean are drugs that have been shown in carefully controlled studies to alleviate much of the discomfort associated with prostate gland overgrowth. Europeans use beta-sitosterol by itself or in combination with saw palmetto to alleviate urinary symptoms of benign prostate enlargement. As the word gets out about the documented benefits of beta-sitosterol, American consumers can expect to see more prostate support products that contain this low-cost plant sterol. Strum: Beta-Sitosterol 2005
Terazosin is prescribed to relax muscles in enlarged prostate and bladder, thereby making it easier to urinate. Also used to lower high blood pressure and prevent strokes.
Finasteride was introduced in the 1990s for the treatment of BPH. It has been shown to reduce DHT in the serum by 70% and in the prostate by up to 90%. Roehrborn: BPH overview 2005
Public uninformed about urine problems: Most males and females are not informed about BPH, symptoms of BPH, evolving urination problems and especially urination retention. Oh, they know "peepee" and "weewee" from childhood, but that is all they needed to know until age 40! Such terminology does not help to describe inability to urinate and other problems needed to communicate with medical doctors. There is a reason why most Americans lack knowledge about the function of their bodies and understanding how their ability to urinate changes as they age. "They never got it when they were young!
So when males have a discussion about urination with their general practitioner [GP], they do not use trigger words that relate their current state of urination in vivid and meaningful "severity of symptoms" words that their GP can interpret. Hence, a brewing BPH problem like the significance of 'urination complaints' goes unrecognized and it's resolution postponed. Medical doctors must confirm the unsophisticated patient comments and validate BPH seriousness [a preventive approach]. In such suspected situations, the GP should recommend cystoscopy; generally considered to be the most specific method with which the urologist evaluates the degree and potential magnitude of urination problem and urethral blockage. Dmochowski: Bladder Outlet Obstruction 2005
It is in a required health education class that such urination information can and should be provided, along with sexually transmitted diseases and body anatomy. Such information could be offered in biology classes, although biology classes do not have time to explain urination problems when coping with the mandatory biology content. Unfortunately, health education is a missing class in most high schools in United States and has been supplanted by shortcut classes like physical education, drug education and sexually transmitted diseases . Those high schools and colleges that do offer courses in health education fail to deal with the emerging urinary problems of men and women in later life. Hence, young persons grow up unaware that they may have urine problems or be able to recognize such problems!
The vested interest video below has suggestions for keeping an enlarged prostate gland in check. You should work with your medical healer on this issue.
Treat an Enlarged Prostate Naturally 2015 Length = 4:11 mns. Click
refresh to activate video
Hope all this information was informative and of help.
References:
Aggarwal Himanshu and Gary E. Lemack, "Primary Bladder Neck Obstruction in Men and Women: an Update on Diagnosis and Management," Current Bladder Dysfunction Reports, September 2015, Volume 10, Issue 3, pp 288-294. Aggarwal: Bladder neck obstruction update 2015
Awad AB, Burr AT, Fin CS., "Effect of resveratrol and beta-sitosterol in combination on reactive oxygen species and prostaglandin release by PC-3 cells," Prostaglandins Leukot Essent Fatty Acids, March 2005;72(3):219-26. Awad: beta-sitosterol & BPH 2005
Bid HK, Konwar R, Singh V. , "Benign prostatic hyperplasia: Is it a growing public health concern for India?" Indian J Med Sci 2008;62:373-4. Bid: BPH concern for India 2008
Dmochowski Roger R., "Bladder Outlet Obstruction: Etiology and Evaluation," Rev Urol., 2005; 7(Suppl 6): S3–S13. Dmochowski: Bladder Outlet Obstruction 2005
Loughlin, Abraham Morgentaler, Martin G. Sanda, "Harvard experts discuss surgical options for benign prostatic hyperplasia," Harvard Review, Originally published April 1, 2007; last reviewed April 26, 2011; 2016. Article by Loughlin: TURP options is no longer active.
Lenard Lane, "New Advances in Natural Prostate Support," Nutrition Review, AUGUST 31, 2014; [NUTRITION REVIEW ARCHIVE, PROSTATE SUPPORT]. Lenard: Natural prostate support 2014
Lephart Edwin D., "Review: Anti-Oxidant and Anti-Aging Properties of Equol in Prostate Health (BPH)," Open Journal of Endocrine and Metabolic Diseases, 2014, Vol.4 No.11. Lephart: Cause of BPH 2014
Manchanda Parmeet Kaur, Aaron J Kibler, Mei Zhang, Janan Ravi, Hemant K Bid, "Vitamin D receptor as a therapeutic target for benign prostatic hyperplasia," 2012; Volume 28 Issue 4; Pages 377-381. Manchanda: Review Vit D therapy for BPH 2012
McVary Kevin T. and other panel members, "American Urilogical Guideline: Management of Benign Prostate Hyperplasia (BPH)," American Urological Association. Article by McVary: Management of BPH is no longer active.
Measuring Symptoms of Prostate Enlargement In order for scientists around the world to evaluate the efficacy of a particular therapy, certain testing standards have been established:
International Prostate Symptom Score [IPSS]: The score is stated as a number that can range from 0 to 35, depending on the severity of lower urinary tract symptoms. The International Prostate Symptom Score also includes a scoring of quality of life as it relates to urinary symptoms.
Maximum urinary flow rate [Qmax]: A measurement to assess the strength of the urinary stream. The maximum urinary flow rate is commonly decreased with benign prostate disease such as BPH (benign prostatic hyperplasia).
Post void residual urine [PVR]: The third test is the amount of residual urine that remains in the bladder after voiding. This is most easily assessed with pre- and post-void ultrasounds of the bladder.
National Association for Continence, "KEGEL EXERCISES," NAFC. NAFC: Kegel exercises
Patel Nishant D. and J. Kellogg Parsons, "Epidemiology and etiology of benign prostatic hyperplasia and bladder outlet obstruction," Indian J Urol. 2014 Apr-Jun; 30(2): 170–176. Patel: Bladder obstruction review 2014
Payne Richard, "Benign Prostatic Hyperplasia: Impact and Treatment Goals," 2016. Article by Payne: BPH treatment is no longer active.
Roehrborn Claus, "Benign Prostatic Hyperplasia: An Overview," Rev Urol. 2005; 7(Suppl 9): S3–S14. Roehrborn: BPH overview 2005
Selner Marissa and Matthew Solan, "Bladder Neck Obstruction," HealthLine, Medically Reviewed by George Krucik, MD MBA on January 26, 2016. Selner: Bladder Neck Obstruction 2016
Strum Srephen B., and William Faloon, "Beta-Sitosterol," Life Extension magazine, June 2005. Strum: Beta-Sitosterol 2005
Thorpe A and D Neal, "Benign prostatic hyperplasia," The Lancet, April 19, 2003, Volume 361, No. 9366, p1359–1367. Thorpe: BPH 2003
The Urology Group, "Greenlight Photoselective Vaporization of the Prostate - PVP Button TURP," 2013. Article by The Urology Group: Greenlight PVP is no longer active.
Vos, Theo; et al., "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010," The Lancet, December 1, 2012, 380 (9859): 2163–2196. Vos: BPH in world 2012
Vuichoud Camille and Kevin R. Loughlin, "Benign prostrtic hyperplasia: epidemiology, economics and evaluation," The Canadian Journal of Urology, International Supplement, October, 2015. Vuichoud: BPH evaluation 2015
World Health Organization, ""WHO Disease and injury country estimates; Disease and injury country estimates - BURDEN OF DISEASE". WHO, November 11, 2009. WHO: BPH estimates 2009
Wikipedia, "Lower urinary tract symptoms." Wiki: LUTS